Hello, my name is Eric BOTS, and I am a practicing optometrist. I help many doctors and their staff efficiently file insurance claims and maximize reimbursement. I know that many practices struggle to get paid, and I am offering a solution to the problem of filing Medicare insurance claims. So where do you begin? Here are four scenarios that you can choose from to ensure that you maximize your insurance reimbursement. You can choose which one is best for you. Scenario number one: This is not the most efficient way to submit claims, but it is easy to access. You're going to utilize a clearinghouse like Gateway or ENSO. These are two that I've used in the past. Some requirements for you and your staff: You must understand how to code and use modifiers. It's slow and inefficient because you have to put the information into their website. You also have to submit secondary insurance claims, resubmit denied claims after researching why they were denied, and then send a bill to the patient for the balance due. You have to hire, train, and maintain a billing person in your office unless you, the doctor, are going to do this yourself. Here are websites and information for the clearinghouses that I mentioned earlier: ENS Ingenix and Gateway. Scenario number two: This is much more efficient. You're going to utilize practice management software and connect to a clearinghouse. You still have to understand coding and modifiers. You're still going to submit claims to secondary insurance and send bills to the patient for the balance due. You will also have to resubmit any denied claims after researching them. You need to hire, train, and maintain a billing person in your office. However, this is efficient because it utilizes practice management software, so you...
Award-winning PDF software





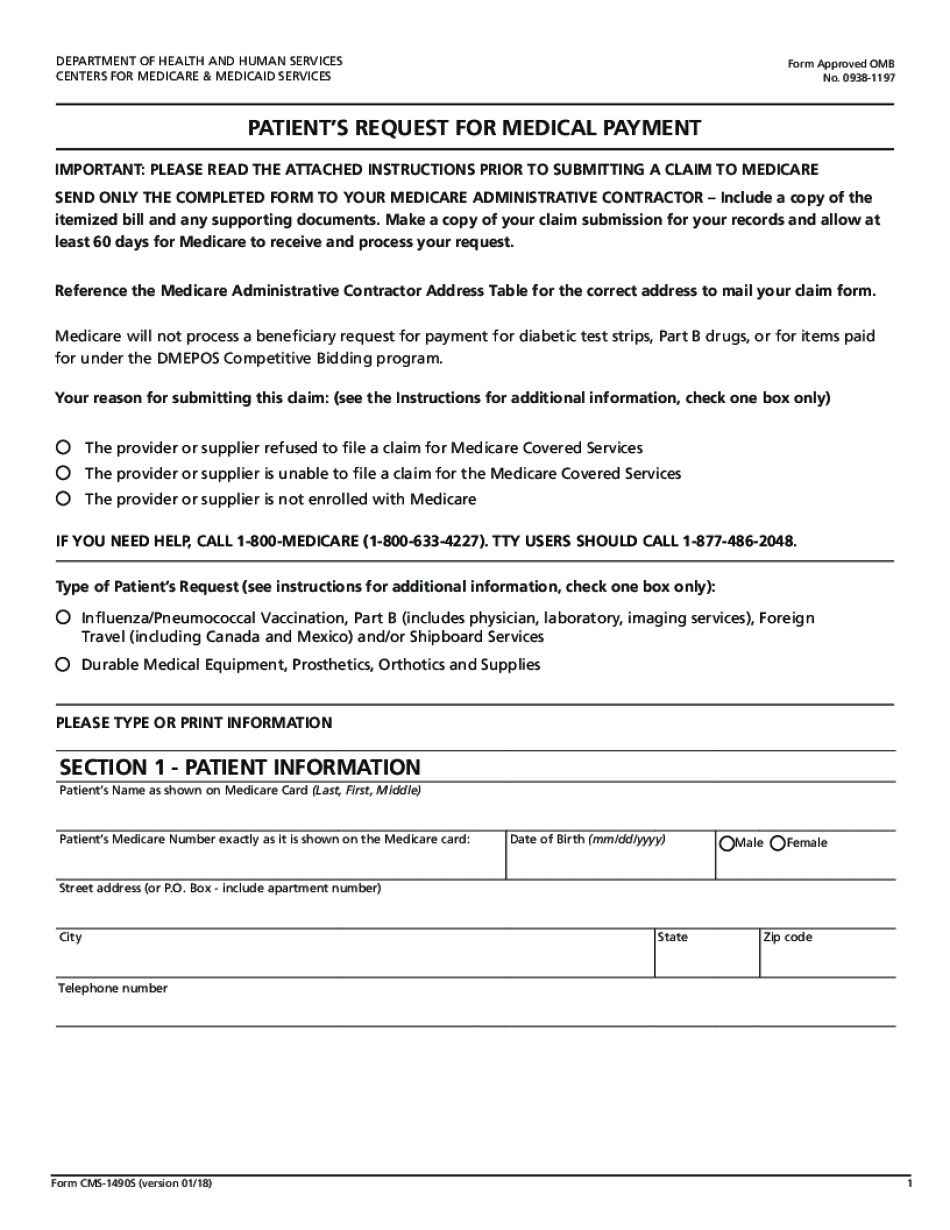
Medicare reconsideration Form: What You Should Know
Appeals Level 2: Public Safety Agency A redetermination is required when you file an appeal to this level of appeal. The appeals level 2 (PSA) is where you file appeal to verify that the Medicare contractor followed its usual procedures for conducting a redetermination, and that this redetermination is justified in order to correct a clerical error. Appeals Level 3: Public Safety Agency For those who believe their claim should have been approved, you can file an appeal at this level of appeal. Public Safety Agencies are responsible for the accuracy of Medicare payments and have power to adjust payments for errors in order to correct a clerical error or clerical error that has been corrected. Appeals Level 4: Feds The Medicare provider must notify this appeals level of appeal to confirm that it has acted in accordance with the CMS regulations. The provider must then follow the CMS guidelines for correcting errors and notifying consumers, and notifies all CMS-covered persons (i.e., Medicaid providers). Any Medicare provider is required to make timely adjustments to Medicare payment if an error was identified or corrected. (There are no public safety agency reviews.) Appeals Level 5: HHS The Medicare provider is also required to notify HHS of any error that occurred with the payment. Appeals Level 6-7: CMS The provider must notify CMS regarding the results of an appeals audit, within 5 days. Appeals Level 8: Medicare Your appeal cannot be determined within the 10-day appeal process (if you are notified of an error, then you will have 20 days to file a claim). If you are granted an appeal, it becomes final and will affect your next determination of eligibility. Appeals Level 9: Other The Medicare provider must notify Medicare of any error and a failure to follow the Medicare Provider Rules Within 3 days of receiving a notice from the Medicare contractor. Any Medicare Provider that fails to abide by the Medicare Provider Rules will be subjected to suspension, penalty, or prosecution and may be required to pay a penalty equal to 25,000 per error. If the provider fails to abide by the Medicare Provider Rules, or if an error is determined to be made out of policy, we will request that the contractor conduct a mandatory appeal process. An official notice of appeal will be mailed to any Medicare account that has received a required notice within 45 days of this initial notice.
online solutions help you to manage your record administration along with raise the efficiency of the workflows. Stick to the fast guide to do Form CMS-1490S, steer clear of blunders along with furnish it in a timely manner:
How to complete any Form CMS-1490S online: - On the site with all the document, click on Begin immediately along with complete for the editor.
- Use your indications to submit established track record areas.
- Add your own info and speak to data.
- Make sure that you enter correct details and numbers throughout suitable areas.
- Very carefully confirm the content of the form as well as grammar along with punctuational.
- Navigate to Support area when you have questions or perhaps handle our assistance team.
- Place an electronic digital unique in your Form CMS-1490S by using Sign Device.
- After the form is fully gone, media Completed.
- Deliver the particular prepared document by way of electronic mail or facsimile, art print it out or perhaps reduce the gadget.
PDF editor permits you to help make changes to your Form CMS-1490S from the internet connected gadget, personalize it based on your requirements, indicator this in electronic format and also disperse differently.
Video instructions and help with filling out and completing Medicare reconsideration form