Let's talk about the newly released pre-authorization rule from Medicare. According to CMS, the OIG, Gao, and cert reports from 2007 and later indicate that documentation errors do not trend toward specific suppliers. However, the root cause of improper payments is a lack of appropriate documentation. What do we know right now about the ruling? CMS estimates that the per case time burden of preauthorization will be the same as for prepayment review, which is 30 minutes per submission. So, where do they come up with the 30-minute guideline? That's because they assume you have all the doctor's notes prior to submitting any claim. We also know that 84 L codes are on the list of potential preauthorization items. Response times, according to the ruling, will be 10 days for an initial submission and 20 days for resubmits. Furthermore, we know that some audit protection will be afforded to claims that have been pre-authorized. Preauthorization will be focused on specific L codes, not on specific suppliers. Therefore, it will be applied to everyone, whether you have a good billing history with Medicare or not. What we don't know right now about the rule is the date for implementation. CMS has published the final rule but has decided not to start implementation yet. They will give a 60-day notice when they come up with a date. We also don't know which of the 84 L codes will be required to have preauthorization. CMS states that they want to implement this rule gradually and will choose only some of the codes. They might also only implement it in certain geographic areas. CMS appears to be on a different page than piano again. Luckily, in the body of the pre-authorization rule, they've provided some insight into their position. I leave you to chew on this quote...
Award-winning PDF software





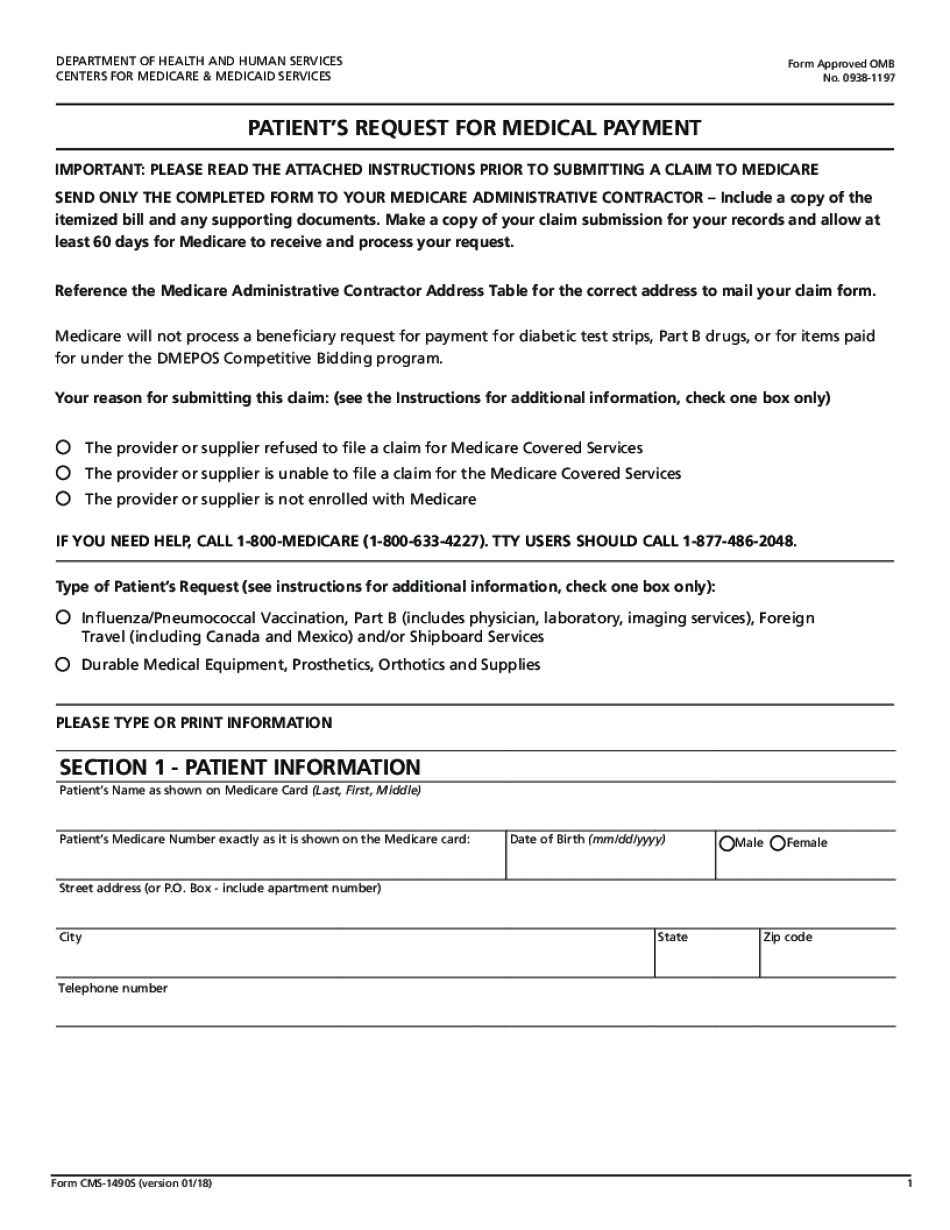
Medicare prior authorization Form: What You Should Know
Medication Prior Authorization Forms for Medicare 7 days ago — Find the Medicare forms and documents you need.
online solutions help you to manage your record administration along with raise the efficiency of the workflows. Stick to the fast guide to do Form CMS-1490S, steer clear of blunders along with furnish it in a timely manner:
How to complete any Form CMS-1490S online: - On the site with all the document, click on Begin immediately along with complete for the editor.
- Use your indications to submit established track record areas.
- Add your own info and speak to data.
- Make sure that you enter correct details and numbers throughout suitable areas.
- Very carefully confirm the content of the form as well as grammar along with punctuational.
- Navigate to Support area when you have questions or perhaps handle our assistance team.
- Place an electronic digital unique in your Form CMS-1490S by using Sign Device.
- After the form is fully gone, media Completed.
- Deliver the particular prepared document by way of electronic mail or facsimile, art print it out or perhaps reduce the gadget.
PDF editor permits you to help make changes to your Form CMS-1490S from the internet connected gadget, personalize it based on your requirements, indicator this in electronic format and also disperse differently.
Video instructions and help with filling out and completing Medicare prior authorization form